
I walk by an eye doctor’s office. The skill of these dedicated professionals to care for such a fragile and sensitive part of the body has always amazed me. Both my sisters wear contact lenses and/or glasses. I wear one contact lens and wear glasses to see distances when I take it out. I used to wear bifocal contacts, but my optometrist switched me to wearing one contact. I love it because now I don’t have to wear reading glasses. I can see to read with just the one contact, and my vision is even better for reading without any contacts or glasses. I just need correction for distance. I have not had surgery on my eyes but had a friend who had LASIK surgery to correct her vision many years ago. It was fairly new at the time but very popular. She was the doctor’s 30th patient of the day. I guess when you get that much practice every day, it really sharpens your surgery skills. Let’s find out more about these sharply skilled medical professionals.

According to Wikipedia, ophthalmology is a branch of medicine and surgery which deals with the diagnosis and treatment of eye disorders. An ophthalmologist is a specialist in ophthalmology. The credentials include a degree in medicine, followed by an additional four to five years of ophthalmology residency training. Ophthalmology residency training programs may require a one-year pre-residency training in internal medicine, pediatrics or general surgery. Additional specialty training or fellowship may be sought in a particular aspect of eye pathology. Ophthalmologists are allowed to use medications to treat eye diseases, implement laser therapy and perform surgery when needed. Ophthalmologists may participate in academic research on the diagnosis and treatment for eye disorders.
Diseases
A partial list of the most common diseases treated by ophthalmologists include those listed below.

Cataracts
A cataract is a cloudy area in the lens of the eye that leads to a decrease in vision. Cataracts often develop slowly and can affect one or both eyes. Symptoms may include faded colors, blurry or double vision, halos around light, trouble with bright lights and trouble seeing at night. This may result in trouble driving, reading or recognizing faces. Poor vision caused by cataracts may also result in an increased risk of falling and depression. Cataracts cause half of all cases of blindness and 33% of visual impairment worldwide.
Cataracts are most commonly due to aging but may also occur due to trauma or radiation exposure, be present from birth or occur following eye surgery for other problems. Risk factors include diabetes, longstanding use of corticosteroid medication, smoking tobacco, prolonged exposure to sunlight and alcohol. The underlying mechanism involves accumulation of clumps of protein or yellow-brown pigment in the lens that reduces transmission of light to the retina at the back of the eye. Diagnosis is by an eye examination.
Prevention includes wearing sunglasses, a wide brimmed hat, eating leafy vegetables and fruits and avoiding smoking. Early on, the symptoms may be improved with glasses. If this does not help, surgery to remove the cloudy lens and replace it with an artificial lens is the only effective treatment. Cataract surgery is not readily available in many countries, and surgery is needed only if the cataracts are causing problems and generally results in an improved quality of life.
About 20 million people worldwide are blind due to cataracts. It is the cause of approximately 5% of blindness in the United States and nearly 60% of blindness in parts of Africa and South America. Blindness from cataracts occurs in about 10 to 40 per 100,000 children in the developing world, and 1 to 4 per 100,000 children in the developed world. Cataracts become more common with age. In the United States, cataracts occur in 68% of those over the age of 80 years. Additionally, they are more common in women and less common in Hispanic and Black people.

Glaucoma
Glaucoma is a group of eye diseases which result in damage to the optic nerve and cause vision loss. The most common type is open-angle (wide angle, chronic simple) glaucoma, in which the drainage angle for fluid within the eye remains open, with less common types including closed-angle (narrow angle, acute congestive) glaucoma and normal-tension glaucoma. Open-angle glaucoma develops slowly over time and there is no pain. Peripheral vision may begin to decrease, followed by central vision, resulting in blindness if not treated. Closed-angle glaucoma can present gradually or suddenly. The sudden presentation may involve severe eye pain, blurred vision, mid-dilated pupil, redness of the eye and nausea. Vision loss from glaucoma, once it has occurred, is permanent. Eyes affected by glaucoma are referred to as being glaucomatous.
Risk factors for glaucoma include increasing age, high pressure in the eye, a family history of glaucoma and use of steroid medication. For eye pressures, a value of greater than 21 mmHg or 2.8 kPa is often used, with higher pressures leading to a greater risk. However, some may have high eye pressure for years and never develop damage. Conversely, optic nerve damage may occur with normal pressure, known as normal-tension glaucoma. The mechanism of open-angle glaucoma is believed to be slow exit of aqueous humor through the trabecular meshwork, while in closed-angle glaucoma the iris blocks the trabecular meshwork. Diagnosis is by a dilated eye examination. Often, the optic nerve shows an abnormal amount of cupping.
If treated early, it is possible to slow or stop the progression of disease with medication, laser treatment or surgery. The goal of these treatments is to decrease eye pressure. A number of different classes of glaucoma medication are available. Laser treatments may be effective in both open-angle and closed-angle glaucoma. A number of types of glaucoma surgeries may be used in people who do not respond sufficiently to other measures. Treatment of closed-angle glaucoma is a medical emergency.
About 70 million people have glaucoma globally. The disease affects about 2 million people in the United States. It occurs more commonly among older people. Closed-angle glaucoma is more common in women. Glaucoma has been called the "silent thief of sight," because the loss of vision usually occurs slowly over a long period of time. Worldwide, glaucoma is the second-leading cause of blindness after cataracts. Cataracts caused 51% of blindness in 2010, while glaucoma caused 8%. The word "glaucoma" is from Ancient Greek glaukos, which means "shimmering." In English, the word was used as early as 1587 but did not become commonly used until after 1850, when the development of the opthalmoscope allowed people to see the optic nerve damage.

Macular degeneration
Macular degeneration — also known as age-related macular degeneration (AMD or ARMD) — is a medical condition which may result in blurred or no vision in the center of the visual field. Early on, there are often no symptoms. Over time, however, some people experience a gradual worsening of vision that may affect one or both eyes. While it does not result in complete blindness, loss of central vision can make it hard to recognize faces, drive, read or perform other activities of daily life. Visual hallucinations may also occur but these do not represent a mental illness.
Macular degeneration typically occurs in older people. Genetic factors and smoking also play a role. It is due to damage to the macula of the retina. Diagnosis is by a complete eye exam. The severity is divided into early, intermediate and late types. The late type is additionally divided into "dry" and "wet" forms with the dry form making up 90% of cases.
Preventive efforts include exercising, eating well and not smoking. There is no cure or treatment that returns vision already lost. In the wet form, anti-VEGF medication injected into the eye or less commonly laser coagulation or photodynamic therapy may slow worsening. Antioxidant vitamins and minerals do not appear to be useful for prevention. However, dietary supplements may slow the progression in those who already have the disease.
In 2015 it affected 6.2 million people globally. In 2013 it was the fourth most common cause of blindness after cataracts, preterm birth and glaucoma. It most commonly occurs in people over the age of 50, and in the United States is the most common cause of vision loss in this age group. About 0.4% of people between 50 and 60 have the disease, while it occurs in 0.7% of people 60 to 70, 2.3% of those 70 to 80 and nearly 12% of people over 80 years old.
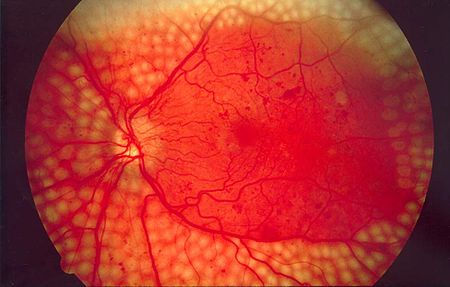
Diabetic retinopathy
Diabetic retinopathy — also known as diabetic eye disease or DED — is a medical condition in which damage occurs to the retina due to diabetes mellitus. It is a leading cause of blindness in developed countries.
Diabetic retinopathy affects up to 80% of those who have had diabetes for 20 years or more. At least 90% of new cases could be reduced with proper treatment and monitoring of the eyes. The longer a person has diabetes, the higher his or her chances of developing diabetic retinopathy. Each year in the United States, diabetic retinopathy accounts for 12% of all new cases of blindness. It is also the leading cause of blindness in people aged 20 to 64.

Dry eye syndrome
Dry eye syndrome or DES — also known as keratoconjunctivitis sicca or KCS — is the condition of having dry eyes. Other associated symptoms include irritation, redness, discharge and easily fatigued eyes. Blurred vision may also occur. The symptoms can range from mild and occasional to severe and continuous. Scarring of the cornea may occur in some cases without treatment.
Dry eye occurs when either the eye does not produce enough ears or when the tears evaporate too quickly. This can result from contact lens use, meibomian gland dysfuction, pregnancy, Sjögren syndrome, vitamin A deficiency, omega-3 fatty acid deficiency, LASIK surgery and certain medications such as antihistamines, some blood pressure medication, hormone replacement therapy and antidepressants. Chronic conjunctivitis such as from tobacco smoke exposure or infection may also lead to the condition. Diagnosis is mostly based on the symptoms, though a number of other tests may be used.
Treatment depends on the underlying cause. Artificial tears are the usual first line treatment. Wrap around glasses that fit close to the face may decrease tear evaporation. Stopping or changing certain medications may help. The medication ciclosporin or steroid eye drops may be used in some cases. Another option is lacrimal plugs that prevent tears from draining from the surface of the eye. Dry eye syndrome occasionally makes wearing contact lenses impossible.
Dry eye syndrome is a common eye disease. It affects 5–34% of people to some degree depending on the population looked at. Among older people it affects up to 70%. In China it affects about 17% of people. The phrase "keratoconjunctivitis sicca" means "dryness of the cornea and conjunctiva" in Latin.

Strabismus
Strabismus is a condition in which the eyes do not properly align with each other when looking at an object. The eye that is focused on an object can alternate. The condition may be present occasionally or constantly. If present during a large part of childhood, it may result in amblyopia or loss of depth perception. If onset is during adulthood, it is more likely to result in double vision.
Strabismus can occur due to muscle dysfunction, farsightedness, problems in the brain, trauma or infections. Risk factors include premature birth, cerebral palsy and a family history of the condition. Types include estropia, where the eyes are crossed ("cross eyed"), exotropia, where the eyes diverge ("lazy eyed" or "wall eyed") and hypertropia where they are vertically misaligned. They can also be classified by whether the problem is present in all directions a person looks (comitant) or varies by direction (incomitant). Diagnosis may be made by observing the light reflecting from the person's eyes and finding that it is not centered on the pupil. Another condition that produces similar symptoms is a cranial nerve disease.
Treatment depends on the type of strabismus and the underlying cause. This may include the use of glasses and possibly surgery. Some types benefit from early surgery. Strabismus occurs in about 2% of children. The term is from the Greek strabismós, meaning "to squint." Other terms for the condition include "squint" and "cast of the eye." "Wall-eye" has been used when the eyes turn away from each other.

Proptosis or bulged eyes
Exophthalmos — also called exophthalmus, exophthalmia, proptosis or exorbitism — is a bulging of the eye anteriorly out of the orbit. Exophthalmos can be either bilateral (as is often seen in Graves’ disease) or unilateral (as is often seen in an orbital tumor). Complete or partial dislocation from the orbit is also possible from trauma or swelling of surrounding tissue resulting from trauma.
In the case of Graves' disease, the displacement of the eye is due to abnormal connective tissue deposition in the orbit and extraocular muscles which can be visualized by CT or MRI.
If left untreated, exophthalmos can cause the eyelids to fail to close during sleep leading to corneal dryness and damage. Another possible complication is a form of redness or irritation called "Superior limbic keratoconjunctivitis," where the area above the cornea becomes inflamed as a result of increased friction when blinking. The process that is causing the displacement of the eye may also compress the optic nerve or ophthalmic artery, leading to blindness.

Excessive tearing or tear duct obstruction
Epiphora is an overflow of tears onto the face, other than caused by normal crying. It is a clinical sign or condition that constitutes insufficient tear film drainage from the eyes, in that tears will drain down the face rather than through the nasolacrimal system.

Uveitis
Uveitis is the inflammation of the uvea, the pigmented layer that lies between the inner retina and the outer fibrous layer composed of the sclera and cornea. The uvea consists of the middle layer of pigmented vascular structures of the eye and includes the iris, ciliary body and choroid. Uveitis is an ophthalmic emergency and requires a thorough examination by an ophthalmologist or optometrist and urgent treatment to control the inflammation. It is often associated with other ocular problems.

Eye tumors
Eye neoplasms can affect all parts of the eye and can be a benign tumor or a malignant cancerous tumor. Eye cancers can be primary (starts within the eye) or metastatic cancer (spread to the eye from another organ). The two most common cancers that spread to the eye from another organ are breast cancer and lung cancer. Other less common sites of origin include the prostate, kidney, thyroid, skin, colon and blood or bone marrow.

History
Ancient Near East and the Greek period
In the Ebers Papyrus from ancient Egypt dating to 1550 BC, a section is devoted to eye diseases.
The pre-Hippocratics largely based their anatomical conceptions of the eye on speculation, rather than empiricism. They recognized the sclera and transparent cornea running flushly as the outer coating of the eye, with an inner layer with pupil and a fluid at the center. It was believed, by Alcamaeon in the 5th century BC, that this fluid was the medium of vision and flowed from the eye to the brain by a tube. Aristotle advanced such ideas with empiricism. He dissected the eyes of animals, and discovering three layers (not two), found that the fluid was of a constant consistency with the lens forming (or congealing) after death, and the surrounding layers were seen to be juxtaposed. He and his contemporaries further put forth the existence of three tubes leading from the eye, not one. One tube from each eye met within the skull.

The Greek physician Rufus of Ephesus (1st century AD) recognized a more modern eye, with conjunctiva extending as a fourth epithelial layer over the eye. Rufus was the first to recognize a two-chambered eye, with one chamber from cornea to lens (filled with water), the other from lens to retina (filled with an egg white-like substance).
Celsus the Greek philosopher of the 2nd century AD gave a detailed description of cataract surgery by the couching method. As a cataract is a clouding in the lens of the eye, couching is a technique whereby the lens is dislodged, thus removing the opacity. Although couching is nowadays routinely practiced only in remote areas in less socially and scientifically countries, it was a precursor to modern cataract surgery and pars plana vitrectom.

The Greek physician Galen in the 2nd century AD remedied some mistakes including the curvature of the cornea and lens, the nature of the optic nerve and the existence of a posterior chamber. Though this model was a roughly correct modern model of the eye, it contained errors. Still, it was not advanced upon again until after Vesalius. A ciliary body was then discovered and the sclera, retina, choroid and cornea were seen to meet at the same point. The two chambers were seen to hold the same fluid, as well as the lens being attached to the choroid. Galen continued the notion of a central canal, but he dissected the optic nerve and saw that it was solid. He mistakenly counted seven optical muscles, one too many. He also knew of the tear ducts.

Ancient India
The Indian surgeon Sushruta wrote “Sushruta Samhita” in Sanskrit in about 6th century CE which describes 76 ocular diseases — of these 51 surgical — as well as several ophthalmological surgical instruments and techniques. His description of cataract surgery was compatible with the method of couching. He has been described as one of the first cataract surgeons.

Medieval Islam
Medieval Islamic Arabic and Persian scientists — unlike their classical predecessors — considered it normal to combine theory and practice, including the crafting of precise instruments, and therefore found it natural to combine the study of the eye with the practical application of that knowledge. Hunayn ibn Ishaq and others — beginning with the medieval Arabic period — taught that the crystalline lens is in the exact center of the eye. This idea was propagated until the end of the 1500s.
Ibn al-Haytham (Alhazen) — in his Book of Optics — explained that vision occurs when light bounces on an object and then is directed to one's eyes.
Ibn al-Nafis, an Arabic native of Damascus, wrote a large textbook, “The Polished Book on Experimental Ophthalmology,” divided into two parts — “On the Theory of Ophthalmology” and “Simple and Compounded Ophthalmic Drugs.”
Avicenna wrote in his Canon "rescheth" which means "retiformis" and Gerard of Cremona translated this around 1150 into the new word "retina."

Modern Period
In the 17th and 18th centuries, hand lenses were used by Malpighi and microscopes by Leeuwenhoek, preparations for fixing the eye for study by Ruysch and later the freezing of the eye by Petit. This allowed for detailed study of the eye and an advanced model. Some mistakes persisted, such as: why the pupil changed size — seen to be vessels of the iris filling with blood, the existence of the posterior chamber and the nature of the retina. Unaware of their functions, Leeuwenhoek noted the existence of photoreceptors, however, they were not properly discovered until Gottfried Reinhold Treviranus in 1834.

Around 1750, Jacques Daviel advocated a new treatment for cataract by extraction instead of the traditional method of couching. Georg Joseph Beer (1763–1821) was an Austrian ophthalmologist and leader of the first Viennese School of Medicine. He introduced a flap operation for treatment of cataracts (Beer's operation), as well as popularizing the instrument used to perform the surgery (Beer's knife).
In North America, indigenous healers treated some eye diseases by rubbing or scraping the eyes or eyelids.

Opthalmic surgery in Great Britain
The first ophthalmic surgeon in Great Britain was John Freke, appointed to the position by the governors of St. Bartholomew’s Hospital in 1727. A major breakthrough came with the appointment of Baron de Wenzel (1724–90), a German who became oculist to King George III of Great Britain in 1772. His skill at removing cataracts legitimized the field. The first dedicated ophthalmic hospital opened in 1805 in London; it is now called Moorfields Eye Hospital. Clinical developments at Moorfields and the founding of the Institute of Ophthalmology — now part of the University College London — by Sir Stewart Duke-Elder established the site as the largest eye hospital in the world and a nexus for ophthalmic research.

19th and 20th centuries
The prominent opticians of the late 19th and early 20th centuries included Ernst Abbe (1840–1905), a co-owner of the Zeiss Jena factories in Germany where he developed numerous optical instruments. Hermann von Helmholtz (1821-1894) was a polymath who made contributions to many fields of science and invented the ophthalmoscope in 1851. They both made theoretical calculations on image formation in optical systems and had also studied the optics of the eye. In Berlin, Albrecht von Graefe introduced iridectomy as a treatment for glaucoma and improved cataract surgery. He is also considered the founding father of the German Ophthalmological Society.

Central Europe
Numerous ophthalmologists fled Germany after 1933 as the Nazis began to persecute those of Jewish descent. A representative leader was Joseph Igersheimer (1879–1965), best known for his discoveries with arsphenamine for the treatment of syphilis. He fled to Turkey in 1933. As one of eight emigrant directors in the Faculty of Medicine at the University of Istanbul, he built a modern clinic and trained students. In 1939, he went to the United States, becoming a professor at Tufts University. German ophthalmologist Gerhard Meyer-Schwickerath is widely credited with developing the predecessor of laser coagulation, photocoagulation. In 1946, he conducted the first experiments on light coagulation. In 1949, he performed the first successful treatment of a retinal detachment with a light beam — light coagulation — with a self-constructed device on the roof of the ophthalmic clinic at the University of Hamburg-Eppendorf.

Polish ophthalmology dates to the 13th century. The Polish Ophthalmological Society was founded in 1911. A representative leader was Adam Zamenhof (1888–1940), who introduced certain diagnostic, surgical and nonsurgical eye care procedures and was shot by the German Nazis in 1940. Zofia Falkowska (1915–93) head of the faculty and Clinic of Ophthalmology in Warsaw from 1963 to 1976, was the first to use lasers in her practice.
Comments